In my years of practice, I’ve encountered nearly every common misconception about weight loss surgery. Patients walk into my clinic with questions like, “Doctor, is it true that I’ll never eat normally again?” or “My friend said everyone just gains the weight back.”
Today, I want to clear up everything about bariatric surgery myths. Let me share what I tell my patients when they come to me confused by all the conflicting information out there.
I wish I had a rupee for every time I’ve heard this one! Here’s what I tell my patients: if you think surgery is easy, you haven’t really understood what we’re doing here.
Look, Mayo Clinic Health System puts it perfectly—bariatric surgery combined with lifestyle changes gives you long-term results that can transform your health. But notice they said “combined with lifestyle changes.” That’s really important.
Before surgery, my patients go through a thorough pre-op preparation . We do medical tests, assess medical and anaesthesist fitness opinion and optimize the present illnesses
After surgery? That’s when the real work begins. You’re committing to a completely new way of eating, exercising regularly, taking vitamins daily, and coming in for follow-ups.
If anything, surgery is the hard way—but it’s the way that actually works when everything else has failed or is not suitable, sometimes even the first choice when appropriate.
I understand this fear. Any surgery sounds scary. But let me share some numbers with you.
Research from the National Institutes of Health shows that bariatric surgery has a mortality rate of less than 0.5%. That’s actually lower than many routine surgeries. We’re talking about a procedure that’s incredibly safe with today’s laparoscopic techniques.
Here’s something even more important: studies tracking patients for up to 40 years found that people who had bariatric surgery had 16% lower death rates overall compared to those who didn’t. Another major study showed a 51% reduction in mortality for surgical patients compared to similar patients who skipped surgery.
Think about it this way—what’s riskier: a proven, safe procedure, or continuing to live with severe obesity and all its complications? As Broward Health points out, bariatric surgery is actually safer than living with untreated severe obesity.
No, no, no. This frustrates me because it undermines the purpose of what we’re doing here.
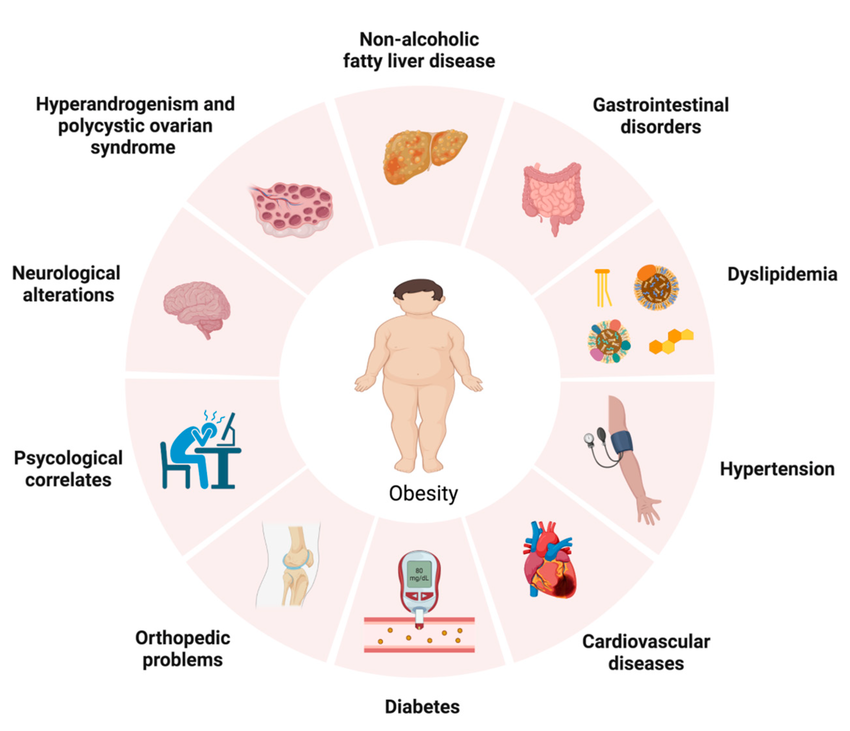
The American Society for Metabolic and Bariatric Surgery makes it crystal clear—these surgeries are medical treatments. We’re treating diabetes, high blood pressure, sleep apnea, high cholesterol, and dozens of other serious conditions.
I’ve had patients come off insulin completely. I’ve seen sleep apnea disappear. Blood pressure normalised. Joint pain gone. These aren’t cosmetic changes—these are life-saving transformations.
Yes, my patients look better afterwards. That’s wonderful! But it’s a side benefit, not the goal. Insurance companies understand this, too and that’s why they cover it as a medical necessity, not as cosmetic work.
This myth really bothers me because it keeps people who could benefit from seeking help. Let me show you the real data.
Yale Medicine reports that more than 90% of bariatric patients maintain long-term weight loss of 50% or more of their excess weight. Ninety per cent!
Do some patients regain some weight? Sure. But “some weight” is very different from “all the weight.” Most patients lose up to 77% of excess weight within the first year and maintain significant losses for years.
In fact, a 2024 review compared bariatric surgery to those new weight loss medications everyone’s talking about. Guess what? Surgery still wins for the greatest and most sustained weight loss.
The patients who struggle are usually those who don’t stick with the program. That’s why I’m so strict about follow-ups and lifestyle commitment.
Actually, you might be surprised. It’s not just about the number on the scale.
Yes, we typically recommend surgery for all for a BMI over 35. But if your BMI is between 30 and 35 and you’re dealing with diabetes, heart disease, or severe sleep apnea, you could be a candidate. Cleveland Clinic references NIH guidelines that recognise how nearly impossible it is for people with severe obesity to lose weight through diet and exercise alone.
Every patient is different. Come talk to me. Let’s look at your whole health picture, not just a number.
This one makes me chuckle because my patients post-surgery often eat healthier and more enjoyably than before!
Yes, the first few months after surgery involve a strict progression—liquids, pureed foods, soft foods, then regular foods. But once you’re healed? You can eat most foods. The difference lies in portion sizes and eating habits.
You’ll eat smaller amounts. You’ll chew more carefully. You’ll focus on protein first, then vegetables, then carbs. But icecream on your birthday? A small portion is fine. Wedding cake? Enjoy a bite or two.
The ASMBS notes that as patients lose weight, they actually feel more energetic and enthusiastic about life. Food becomes fuel and occasional pleasure, not an obsession.
My patients tell me they actually enjoy eating more now because they’re not compulsively overeating or feeling sick afterwards.
This is a fair concern, and it’s why we monitor you so carefully.
Some procedures do affect how you absorb nutrients. That’s why every single one of my patients takes daily vitamins and comes in for regular blood work. When we catch deficiencies early (and we do, because we’re checking), they’re easy to correct with supplements.
Is it an inconvenience? Maybe a small one. But diabetes medication, blood pressure pills, CPAP machines—those are inconveniences too. I’d rather have you taking a few vitamins than dealing with a heart attack.
I use laparoscopic techniques, which means tiny incisions. We’re talking about 4-5 small cuts, each less than a centimetre. Most patients tell me their scars fade so much that even they forget where they are.
No large incisions. No long recovery. Most people are back to light activity within a week or two.
I wish this were true, but I’d be lying to you if I said it was.
What bariatric surgery does is remarkable. Mayo Clinic research shows it has the most consistent data among all obesity treatments for improving health. Your diabetes might go into remission. Your blood pressure might normalise. Your joints will hurt less.
This one genuinely upsets me because it’s so unfair and wrong.
Obesity is a disease. Cleveland Clinic, citing NIH research, confirms that severe obesity cannot be sustainably managed through willpower alone. We’re talking about genetics, hormones, metabolism, brain chemistry, environment—dozens of factors beyond anyone’s control.
If willpower were effective, wouldn’t my patients have already used it? These are people who’ve tried every diet out there. They’ve lost weight and gained it back more times than they can count. They’re exhausted and desperate.
Bariatric surgery isn’t giving up. It’s using medical science to address a medical problem. We don’t tell diabetics they lack willpower when they need insulin. We don’t blame heart attack patients for needing stents. Why should obesity be different?
Mostly, yes. But in carefully selected cases, we do perform bariatric surgery on adolescents with severe obesity and serious health complications. The criteria are much stricter, and we involve pediatric specialists, psychologists, and the whole family.
These are rare cases, but when a 16-year-old has type 2 diabetes, sleep apnea, and can’t walk up stairs without pain, surgery might be the most compassionate option.
No—I’m restructuring your digestive system. We’re not doing liposuction here. The surgery changes how much you can eat or how nutrients are absorbed there by creating hormonal changes, which causes weight loss over time.
Actually, it’s the opposite! The ASMBS reports that patients feel more energetic after losing weight, with less pain and more enthusiasm for activities. I encourage light walking within days of surgery, and most patients are more active than they’ve been in years.
Despite all this evidence, research in Mayo Clinic Proceedings shows that bariatric surgery is dramatically underused. One big reason? Myths like these create knowledge gaps, even among doctors, leading to low referral rates.
People who could benefit are staying away because of misinformation. That breaks my heart.
If you’re struggling with obesity and related health problems, don’t let myths keep you from exploring your options. Bariatric surgery isn’t perfect, and it’s not for everyone. But it’s a proven, safe, effective medical treatment that has transformed countless lives.
Come talk to me. Ask questions. Challenge my answers. Look at the research. Talk to my patients. Make an informed decision based on facts, not fear.
You deserve accurate information and compassionate care. That’s what I’m here to provide.
Dr. Kedar Patil is a Robotic Bariatric and Laparoscopic Surgeon practicing in Pune. For consultations or more information about whether weight loss surgery might be right for you, please reach out to our clinic.
Disclaimer: This blog is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider about your individual health needs.